Tag: apple health
Changes to Continuous Eligibility for Kids Under Age Six
In April 2023, the Centers for Medicare & Medicaid Services (CMS) approved Washington’s 1115 Waiver request to extend continuous eligibility for any child under six who is enrolled in a free Apple Health (Medicaid) program.
Children under the age of six on free Apple Health will now receive continuous eligibility through their sixth birthday, regardless of changes in household income, if they were eligible in the month of application.
Note: There have been no changes to continuous eligibility for kids over age six on free Apple Health or for those on Apple Health for Kids with premiums, also known as Children Health Insurance Program (CHIP). Coverage for these groups continues to be renewed for 12 months at a time.
What is being done to keep kids covered?
In June 2023, the Health Care Authority (HCA) began work to maintain continuous eligibility for children under the age of six. A manual process is in place to identify eligible children who have lost coverage and reinstate them.
Once the system supports continuous eligibility for kids under age six, children who are active on free Apple Health Kids and meet the eligibility criteria will have their certification period automatically extended through the month they turn six.
Apple Health (Medicaid) Renewal Letters Have Begun Mailing
Some clients will automatically renew; and others will need to update their information
OLYMPIA – The Washington State Health Care Authority (HCA), Washington Health Benefit Exchange (Exchange), and the Department of Social and Health Services (DSHS) have begun mailing letters to Washington Apple Health (Medicaid) clients reminding them to update their contact information and renew coverage to see if they still qualify.
For the first time in over three years, people on Apple Health could lose coverage if their family income has gone up. Federal requirements during the COVID-19 public health emergency (PHE) led to income checks being suspended to keep clients enrolled in Apple Health during the pandemic. However, last December’s federal omnibus spending bill directed states to resume evaluating eligibility of Medicaid enrollees on April 1 to wind down COVID-19 pandemic emergency measures.
Washington has until April 2024 to process eligibility redeterminations for all 2.3 million Apple Health clients. It’s the largest benefit renewal process the state has ever attempted. Here is what you need to know during this effort.
How the renewal process works
Washingtonians on Apple Health will get their renewal notifications at different times. To manage the workload, the renewals are being spread out over the next 12 months.
Some clients will be automatically renewed based on the most recent information already on file with the state. If the state does not have enough information on file, clients will need to take action to complete the renewal process to stay insured.
- If clients are auto renewed, they will get a notification saying their health coverage was renewed. For most, health coverage will be renewed for 12 months. The requirement will continue for clients to report any changes within 30 days.
- If clients are not auto renewed, they will get a renewal notice in the mail. They must respond to complete their renewal by the 60-day deadline. If at the end of 60 days the client hasn’t responded, the state will send a notice informing them their Apple Health benefits are ending.
How to know when it’s time to renew
Your renewal month typically matches the month your Apple Health coverage started. Clients can check their most recent Apple Health notice to confirm their renewal date. The month before their renewal date, clients will receive a notice about their Apple Health renewal. For example, if a client’s coverage is up for renewal on May 31, 2023, they should act now to avoid a loss in coverage.
Starting April 2023 through March 2024, HCA and DSHS will evaluate current Apple Health client eligibility for continued coverage and renew or terminate coverage as appropriate.
What steps do clients need to take?
We encourage Apple Health clients to take the following steps:
- Update their contact information as soon as possible.
- Check their mail or email. Starting in April and through March 2024, clients will receive information about their Apple Health coverage via mail or email. This notification may require them to take action in order to maintain coverage.
- Complete their renewal by the deadline on their notice.
“It’s imperative that Washingtonians enrolled in Apple Health take time to update their contact information to ensure they receive upcoming notices related to their health care coverage,” said Sue Birch, HCA director. “If people learn they are no longer eligible for Apple Health, there are other options for low-cost health coverage.”
“We know how important it is to have access to health care when we need it most, and we are committed to making sure people stay connected to this vital benefit,” said Jilma Meneses, DSHS secretary. “We are ready to answer any questions or concerns people might have, and to provide as seamless a process as possible.”
“We want to ensure all Washingtonians stay covered, whether it is Apple Health, employer sponsored, or a new qualified health plan,” said Ingrid Ulrey, CEO at Washington Health Benefit Exchange powering Washington Healthplanfinder. “If you receive a letter from HCA, Washington Healthplanfinder, or DSHS, make sure you open it, and visit Healthplanfinder right away so we can help you with your insurance needs. For those who are now above income eligibility, they will have the opportunity to enroll in high-value, low-cost Cascade Care Plans, now available for as low as $10 or less per month.”
To help Washingtonians transition to other health insurance, HCA has partnered with DSHS and Washington Healthplanfinder to connect people to other coverage. To ensure clients receive important notices about their health care coverage, including other coverage options, Apple Health clients can update their contact information using one of the following options:
- For single adults, children, pregnant individuals, and parents/caretakers:
- Online: wahealthplanfinder.org or download the WAPlanfinder app
- Phone: 1-855-923-4633
- For individuals who are aged, have blindness or a disability, or are eligible for Medicare:
- Online: washingtonconnection.org
- Phone: 1-877-501-2233
Your Apple Health: What you need to know about the Public Health Emergency
During the Covid-19 Public Health Emergency, Washington State changed some rules about Apple Health (Medicaid). If you or a family member had Medicaid for health insurance, you did not have to renew every year. If you paid a premium for Medicaid health insurance, premium payments stopped during the Public Health Emergency. Some people received temporary health insurance coverage if they qualified for other benefits.
The PHE ended March 31, 2023, and now:
- Beginning April 2023, you must renew your Apple Health/Medicaid insurance
- If you usually paid a premium, premiums are starting up again
- You may need a new eligibility review
If you do not renew, do not complete a required eligibility review or if you do not pay a premium when it is due, you may lose your health insurance coverage for you or your family member.
What to do:
- Update your contact information with your insurance provider so your provider can send you important information about renewal, eligibility reviews and premiums
- Renew your insurance when your provider tells you
- Premiums for certain Apple Health/Medicaid insurance plans are starting again (Apple Health for Kids with premiums/Children’s Health Insurance Program, Apple Health for Workers with Disabilities (HWD). Watch your mail or email for notices or premium bills from your provider
If you are on one of these Apple Health/Medicaid plans, call:
- Amerigroup: 1-800-600-4441
- Community Health Plan of Washington: 1-800-440-1561
- Coordinated Care: 1-877-644-4613
- Molina:1-800-869-7165
- UnitedHealthcare: 1-877-542-8997
If you usually get notices from WA State Health Care Authority email askmedicaid@hca.wa.gov with your name, date of birth, and updated contact information.
If you usually get notices from Washington Healthplanfinder:
- Log in to your Washington Healthplanfinder account at wahealthplanfinder.org
- Call Washington Healthplanfinder at 1-855-923-4633
If you are age 65 and older, have blindness or a disability, get Medicare, and get healthcare coverage through Department of Social and Health Services (DSHS):
- Update contact information at waconnection.org or call 1-877-501-2233 or
- Visit your local Community Service Office
Medicare Advantage Special Needs Plans for dual eligible (Medicare and Medicaid) clients
Medicare Advantage Special Needs Plans are available to clients who are eligible for Medicare and Medicaid (dual eligible). Special Needs Plans provide additional benefits to clients beyond what traditional Medicare and Medicaid provide including, but not limited to, care coordination, gym memberships, transportation to medical appointments and meal delivery.
Click the below link to learn more.
What You Can Do to Help Kids Stay on Medicaid in 2023
One of the few silver linings of our bleak public health reality throughout the COVID-19 pandemic is that child health insurance coverage under Medicaid and the Children’s Health Insurance Program (CHIP) is at an all-time high. Due to temporary protections against Medicaid disenrollment, about 41 million children are insured through Medicaid or CHIP as of August 2022–greater than the population of California.
The long-term benefits of Medicaid enrollment on the health and wellbeing of children–particularly young children between the ages of 0 and 3–are well documented. Medicaid covers half of all babies born in the United States, which is 40 percent of all children. Study after study has shown that childhood Medicaid coverage is associated with long-lasting benefits to overall health, educational attainment, and financial stability.
However, temporary continuous coverage protections originally implemented as part of the COVID-19 pandemic response will end on March 31, 2023. This means that states will resume normal Medicaid renewal processes for all enrollees. Specifically, states will disenroll people who don’t complete the process or are newly ineligible for coverage. Policy advocates estimate that more than 6.7 million children are at risk of losing coverage if there is not a collective effort to ensure that all eligible children remain enrolled in Medicaid. State administrators, service providers, advocates, and parents/caregivers must all take proactive steps to ensure that children are not improperly disenrolled from Medicaid when states begin the massive administrative undertaking of restarting the re-enrollment process in the coming months.
Read the full article from the Center for Law and Social Policy.
Moving ForWArd: Join us and become an Apple Health Ambassador today!
The Health Care Authority (HCA) needs you! In preparation for the end of the public health emergency (PHE), we are looking for volunteers to share Apple Health (Medicaid) information with their community. Let’s help keep Washingtonians covered!
Get involved!
Many times, people from our community have difficulties accessing Apple Health programs and services due to language barriers, transportation, lack of engagement, etc. We are looking for volunteers from organizations such as schools, food banks, churches, and community advocates to get involved and become an Apple Health Ambassador.
If you or someone you know would like to participate contact AHEligCovid19@hca.wa.gov.
Resources
HCA will continue to share updates as new information becomes available. Follow us on social media for updates on Apple Health. For more information about the Public Health Emergency visit hca.wa.gov/phe.
Care Coordinators: MCOs’ Best Kept Secret
For families who have children with complex health care needs, coordinating all the appointments, medications, and therapies can be difficult. When an individual has several doctors and specialists that they regularly see, the help of a care coordinator can be invaluable. A care coordinator, or patient care coordinator, is a health professional employed by an MCO, or managed care organization, to oversee complex care cases. They can help with getting needed appointments, acquiring resources outside of prescriptions, ensuring that medications are easily available and do not have any interactions, and help families have better peace of mind that all of their medical practitioners are on the same page.
Care coordinators are available to many patients, but they are rarely given as an option to overtaxed patients or patients’ parents. Primary care physicians sometimes recommend a care coordinator to help a patient or family, but as they are not familiar with every aspect of a patient’s life and health care, they will often assume that a family does not need a care coordinator when they would be greatly aided by having one. For those with a strong connection to a primary provider, asking them to request a care coordinator for their healthcare can be an efficient way to start the process. While a primary care physician is often the one to initiate the assistance of a care coordinator, is possible for a patient or their family to request care coordination on their own.
The process for requesting a care coordinator is different through different health care systems. The majority of individuals on Medicaid, also known as Apple Health, have their healthcare covered by an MCO. Calling the MCO’s customer service line is often the first step in getting a care coordinator. The phone numbers of the five MCO’s that oversee apple health in Washington state are as follows: Amerigroup at 1-800-600-4441, Community Health Plan of Washington at 1-800-440-1561, Coordinated Care of Washington at 1-877-644-4613, Molina Healthcare of Washington at 1-800-869-7165, and UnitedHealthcare Community Plan at 1-877-542-8997. If you are unsure which MCO is in charge of your healthcare, view our video on Who is in Charge of Your Apple Health Healthcare? If there are problems in getting through to your MCO, you can call the Health Care Authority, that oversees all Washington Medicaid MCOs, at 1-800-562-3022.
Who is in Charge of Your Apple Health Healthcare?
For individuals enrolled In Washington State Medicaid, also known as Apple Health, understanding who manages their medical care is not always easy. In almost all cases, the management of care for people with Apple Health is delegated to an MCO, or Managed Care Organization. These are large for-profit organizations that often have a large infrastructure, making it confusing and difficult to find information or direction.
There are five MCO’s under Apple Health in Washington. They are Amerigroup Washington, Community Health Plan of Washington, Coordinated Care of Washington, Molina Healthcare of Washington, and UnitedHealthcare Community Plan. All of these MCOs are available statewide, except UnitedHealthcare Community Plan, with is only available in the western half of the State. For anyone in the foster care system, they are automatically enrolled in Coordinated Care of Washington and this coverage will follow them until they are 21. Health Care Authority has a Service Area Matrix to view what MCOs are available in each county.
Under some circumstances a person on Apple Health will not be put into an MCO. If an individual is American Indian/Alaska Native they can view their options on the Health Care Authority’s American Indians and Alaska Natives page. Other non-MCO Apple Health patients will have a distinct services card that looks the card shown:
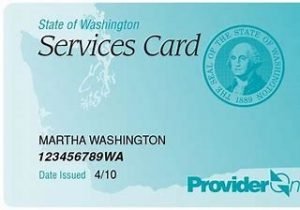
For those patients, review the Health Care Authority’s Handbook on Coverage Without a Managed Care Plan for information about how to receive services. It is also possible to call them at 1-800-562-3022.
For those who do not remember which MCO they or their children are signed up with, it might have been done automatically for them when the initial roll out happened in 2014 or when they first became eligible for Apple Health under the ACA. The switch to managed care was fully implemented in 2020. Here are three ways in which to find out which MCO is overseeing an individual’s care:
- Review your Provider One Card to see which MCO is listed. Individuals who are on MCO-managed Apple Health will have the name and/or logo of the MCO on the Provider One card, like the example
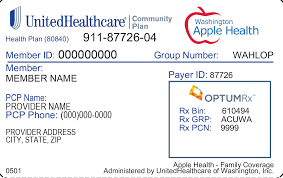
In this case, UnitedHealthcare is the MCO. The PCP listed is the Primary Care Physician, or a patient’s main doctor, and the PCP phone number listed can be called to schedule visits and ask medical-related questions.
- If the provider card is missing, call: 1-800-562-3022 and choose option 1 for self-service, then option 1 for services card. They can help replace the provider card and help enrollees get the services they require.
- Call the Health Care Authority Customer Service Line at 1-800-562-3022.
It is important to note that everyone enrolled in Apple Health within one household must be on the same managed care plan. Provider One cards are usually sent out once a year to enrollees and there is a number on the card to call for customer service. Below is the Apple Health managed care plan contact information:
| Amerigroup (AMG) | 1-800-600-4441 |
| Community Health Plan of Washington (CHPW) | 1-800-440-1561 |
| Coordinated Care of Washington (CCW) | 1-877-644-4613 |
| Molina Healthcare of Washington, Inc. (MHW) | 1-800-869-7165 |
| UnitedHealthcare Community Plan (UHC) | 1-877-542-8997 |
All Apple Health enrollees have the right to change their MCO at any time, with no fee and with no gap in coverage. The shift usually occurs by the 15 of the following month, but the Provider One portal can help if there are challenges. There are several ways to switch plans:
- Visit the Washington Healthplanfinder
- Visit the ProviderOne Client Portal website.
- Call the Health Care Authority at 1-800-562-3022 (TRS: 711).
If considering changing to a different MCO, visiting other MCOs websites or calling their information line with some questions can be useful. It is helpful to see what hospitals, urgent care facilities, specialists, and therapists are covered. Not all physicians or medical facilities that take Apple Health are contracted with all MCOs.
View our video on Who is in Charge of Your Apple Health Healthcare?

